Background:
Mantle cell lymphoma (MCL) is a rare, often aggressive type of B-cell lymphoma with poor survival and no cure. Cancer and cancer treatment has a negative impact on health-related quality of life (HRQOL) both during active disease and in the long term, and improvement of HRQOL may be one of the most important objectives of cancer therapy. In addition, baseline HRQOL has in other lymphoma populations been shown to be predictive of outcome. Hitherto, there are only few reports on HRQOL in MCL. The primary aim of this study was to explore HRQOL before, during and after chemotherapy in an elderly population with MCL. Secondary aims were to identify predictors for HRQOL, information that can be used for improvement in rehabilitation.
Methods:
The cohort consisted of patients included in the multicenter open-label phase Ib-II NLG-MCL4 trial (LENA-BERIT), designed to evaluate the addition of lenalidomide (LEN) to rituximab-bendamustine (R-B) as first-line treatment in elderly patients (>65 years) with MCL. The treatment with R-B stopped after six months, LEN continued for six more months. HRQOL was assessed by the EORTC QLQ-C30 questionnaire pre-treatment, and after 6, 12 and 24 months post study inclusion. For the functional scales and the global quality of life scale a higher score represents a better level of functioning. For the symtom scales and single items, a higher score corresponds to a higher level of symtoms. Patient scores were compared to scores from a reference population sample at baseline. Survival was analysed by Kaplan-Meier estimates, and cox regression multivariate analysis was used to assess survival with adjustments for prognostic factors, age, sex and more.
Results:
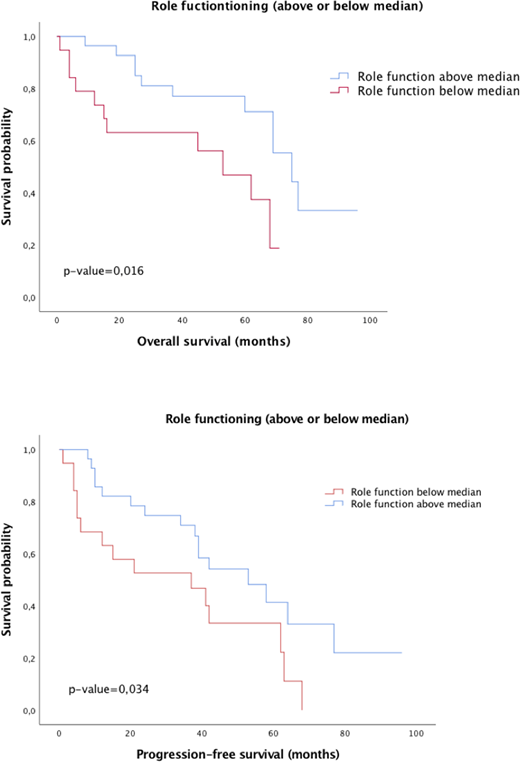
Fifty-one patients were enrolled, 1 patient was excluded based on screen failure. Median age was 71 years (range 62-84), 37 were men (73%). Stratified according to Mantle Cell Lymphoma International Prognostic Index (MIPI), 5 (10%) were low-risk, 18 (38%) intermediate and 26 (52%) high-risk. Follow-up time for living patients were 52 months, and for deceased patients 27 months. Median overall survival time were 52 months. The proportion of patients reporting HRQOL data was at baseline; 48 (96%), after 6 months; 33 (83%), after 12 months; 27 (89%), and after 24 months; 12 (75%). During the first six months of treatment, several functional scores deteriorated, and after 12 months it had stabilised at baseline level or better. The global health status (QoL) improved at 12 months after diagnosis, but then dropped to baseline levels after 2 years. Before treatment, patients exhibited levels of the symptom scores, comparable to the reference population. Six months after start of therapy, the scores for pain, dyspnoea and insomnia were improved, while appetite loss and diarrhoea were impaired. After 12 months, the symptom scales improved to a level superior compared both to baseline and the reference population. The population was divided into two groups, with the median as cut-off values. In the multivariate analysis, including MIPI, gender and the presence of TP53 mutation, impaired pre-treatment physical function, role function and elevated pain score were independent prognostic markers for overall survival. Role function and pain were also independent prognostic markers for progression free survival.
Conclusion:
In this population of elderly patients with MCL, pre-treatment HRQOL was similar to the reference population. During treatment, HRQOL deteriorated, but reverted to the same level as the reference population after treatment. Pre-treatment physical and role function and pain were independent factors associated with overall survival. These novel findings may be used to design support during treatment and improve rehabilitation.
Jerkeman:Roche: Research Funding; Celgene: Research Funding; Janssen: Research Funding; Gilead: Research Funding; Abbvie: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.